Explore various treatment choices available for managing hiatus hernia, including surgical and non-surgical approaches.
Dr Ahmed Hassn is Best Laparoscopic & Bariatric Surgeon in Dubai recognised for his exceptional and major contribution to the surgery of GERD and hiatus hernia. He regularly receives referrals from other surgeons in the country for complex hiatus hernia and for previously failed surgery.
He has performed more than one thousand laparoscopic antireflux surgery with excellent outcomes.
He has published extensively on antireflux surgery, hiatus hernia repairs and on redo antireflux surgery for failed procedures.

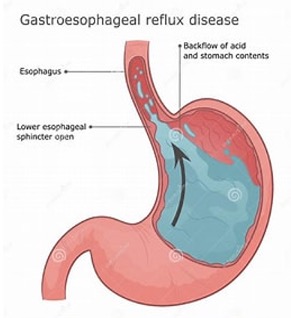
Acid is secreted in the stomach to help the digestion of food and to kill many harmful compounds. The stomach lining is adapted to this acid, but the lining of the gullet (esophagus) is not adapted to acid.
We all have a valve mechanism at the lower part of the gullet (LES) which allows food to go down to the stomach but prevents acid and other stomach contents from regurgitating to the gullet.
When this valve is weakened or in association with a hiatus hernia, acid and other contents of the stomach regurgitate back to the gullet and cause symptoms and if left untreated, it can cause permanent damage to the gullet.
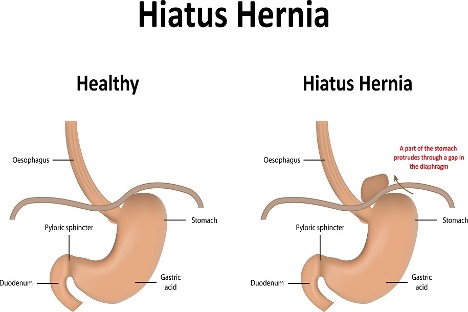
Hiatus Hernia is a condition that occurs when a part of the stomach protrudes through the diaphragm into the chest cavity. This can weaken the lower esophageal sphincter (LES), the muscle that normally prevents stomach acid from flowing back into the esophagus. Hiatus Hernia can lead to GERD, causing heartburn, regurgitation, chest pain, and other uncomfortable symptoms.
Other symptoms may include:
Hiatus Hernia & Anti Reflux Surgery and GERD are not synonymous but there is a common association. Not every patient with reflux would have a Hiatus Hernia & Anti Reflux Surgery not every patient with a hiatus hernia would have reflux.
Hiatus Hernia & Anti Reflux Surgery remain to be the only definitive treatment to cure GERD. During surgery, the LES is reinforced to prevent acid reflux and alleviate the symptoms associated with GERD. The surgery can significantly improve the patient’s quality of life by reducing the need for long-term medication use and minimizing GERD-related complications.
Before Hiatus Hernia & Anti Reflux Surgery, a thorough evaluation is necessary to determine the patient’s candidacy and to tailor the treatment plan to their specific needs. The preoperative evaluation may include:
In some cases, other tests might be required if the diagnosis was not established by the above tests.
Hiatus Hernia & Anti Reflux Surgery is commonly performed using a minimally invasive technique called laparoscopy. During the procedure, the surgeon creates a new and tighter valve mechanism around the lower esophagus to prevent reflux. This can be achieved through various surgical approaches. Nissen fundoplication is the gold standard treatment. Laparoscopy offers several benefits, including smaller incisions, reduced scarring, faster recovery, and a shorter hospital stay.

This is a relatively new entity where a percentage of patients who had sleeve gastrectomy might develop GERD.
Those patients whom their symptoms are not controlled by medical treatment might require surgical treatment. The most used procedures include laparoscopic repair of the Hiatus Hernia & Anti Reflux Surgery (diaphragm muscles) or laparoscopic modification of the previously sleeved stomach.
Dr Ahmed Hassn is a UK trained highly qualified Best Laparoscopic & Bariatric Surgeon with more than 21 years of consultant experience in his field.
Don’t miss our future updates! Get Subscribed Today!
©2024. Dr Ahmed Hassn. All Rights Reserved.